3.2
Impact Factor
ISSN: 1837-9664
J Cancer 2024; 15(1):140-148. doi:10.7150/jca.89715 This issue Cite
Research Paper
Prevalence of cervical precancers or cancers in women with ASC-H/HSIL cytology according to Aptima HPV (AHPV) assay-detected HPV genotypes and age
1. Departments of Pathology, International Peace Maternity and Child Health Hospital Affiliated to Shanghai Jiao Tong University School of Medicine, Shanghai, 200030, China.
2. Department of Pathology, Zhejiang University School of Medicine Women's Hospital, Hangzhou, Zhejiang Province, 310006, China.
3. Department of Gynecology, Zhejiang University School of Medicine Women's Hospital, Hangzhou, Zhejiang Province, 310006, China.
4. Department of Pathology, University of Texas Southwestern Medical Center, Dallas, TX, 75390, USA.
5. Department of Pathology, Parkland Hospital, Dallas, TX, 75235, USA.
* Q.L. and L.C. contributed equally.
Abstract
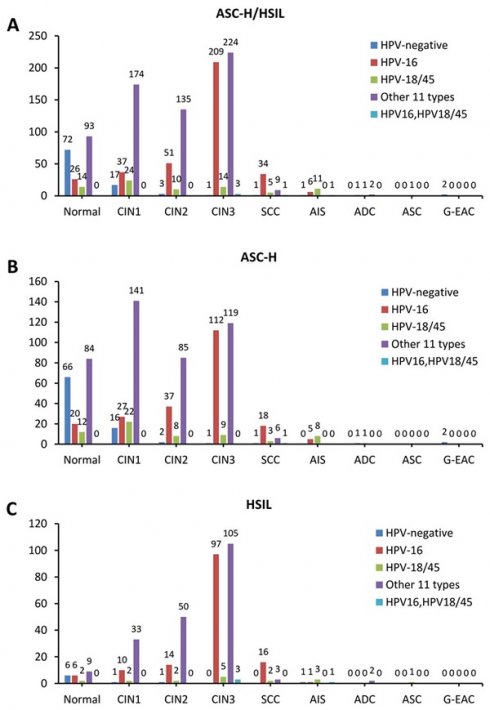
Objective: Aimed to potentially risk-stratify patients with different cervical cytology diagnoses, by HPV genotypes and/or age, we have conducted a series of studies to examine the prevalence of cervical precancers and cancers for women with different cytology diagnoses. This paper will be focusing on patients with ASC-H/HSIL cytology.
Methods: In total, 1183 patients aged 20-78 years with atypical squamous cells, cannot rule out HSIL (ASC-H)/HSIL by cytology underwent AHPV assay and cervical biopsy in a developed region in southern China were included in this study.
Results: Overall, 59.2% women with ASC-H/HSIL cytology had cervical intraepithelial neoplasia (CIN)2/3 lesions while 1.6% had adenocarcinoma in situ (AIS) lesions. Compared to other groups, HPV-16+ group (80.8%) showed a significantly higher prevalence of CIN2/3 than other genotype+ groups (p<0.0001). Further, HPV-16+ (9.3%) or HPV-18/45+ (6.3%) group showed a significantly higher prevalence of squamous cell carcinoma (SCC) than other genotype+ groups (p<0.0001). The prevalence of AIS glandular lesions in HPV-18/45+ group (13.8%) is significantly higher than other genotype groups (p<0.0001). When stratified by age, younger group showed a significantly higher prevalence of CIN2/3 (p=0.009) while older group presented an obvious higher prevalence of SCC (p<0.0001).
Conclusions: In this patient population, among women with ASC-H/HSIL cytology, HPV positive groups are at significantly higher risk of CIN2/3 compared to HPV negative group. Specifically, prevalence of CIN2/3 and SCC is significantly higher in HPV-16+ group while AIS lesions are more prevalent among HPV-18/45+ patients. In addition, younger group showed a significantly higher prevalence of CIN2/3 while older group presented an obvious higher prevalence of SCC.
Keywords: risk stratification, E6/E7 mRNA genotyping, ASC-H, HSIL, hrHPV

 Global reach, higher impact
Global reach, higher impact