3.2
Impact Factor
ISSN: 1837-9664
J Cancer 2023; 14(6):981-988. doi:10.7150/jca.82909 This issue Cite
Research Paper
Study on the application of 3D printing head film fixation technology in cranial radiotherapy
1. Department of Radiation Oncology, Hebei Province Cangzhou Hospital of Integrated Traditional and Western Medicine, Cangzhou Hebei, 061000, China.
2. Key Laboratory of Endocrinology of National Health Commission, Department of Endocrinology, State Key Laboratory of Complex Severe and Rare Diseases, Peking Union Medical College Hospital, Chinese Academy of Medical Science and Peking Union Medical College, Beijing, 100730, China.
* These authors contributed equally to this work.
# These authors contributed equally to this work.
Abstract
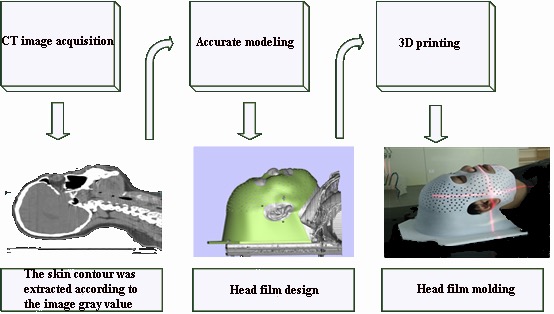
Objective: To investigate the use of 3D printing technology to customize individualized precise radiotherapy head masks for cranial radiotherapy patients. Through the comparison with thermoplastic head film, evaluate the effect of this material on deep dose attenuation and body surface dose, and evaluate its positioning accuracy and repeatability for clinical application.
Methods: Thirty patients with head and neck radiotherapy were divided into the control group and the experimental group. The control group used the traditional thermoplastic head film fixation technique for body position fixation, and the experimental group used the 3D printing head film fixation technique. The patient setup was verified by kV-CBCT scanning to obtain the translational setup error and rotational setup error in the X, Y, and Z directions.
Results: At a depth of 5 cm, both materials have a radiation attenuation rate of <1%. At the surface location, the body surface dose of control group increased by approximately 27%. With a 3D printing head film, the body surface dose increased by approximately 18%. The positioning of two groups of patients was verified by the kV-CBCT, and a total of 232 data sets were obtained. The average translation positioning errors in the X, Y, and Z direction of control group and experimental group were 1.29 mm, 1.42 mm, 1.38 mm and 1.16 mm, 1.24 mm, 1.16 mm, respectively. The average rotation positioning error in the X, Y, and Z direction of control group and experimental group were 1.29°, 1.02°, 1.01° and 1.08°, 0.96°, 1.00°, respectively. The translational setup errors in the Y and Z directions and rotational setup errors in the X direction significantly differed between the control and experimental groups (all p<0.05), but no statistical significance was found in the other directions (all p>0. 05).
Conclusion: Compared to the traditional thermoplastic head membranes, 3D printing head membranes has shown a reliable and reproducible interactional positioning accuracy. Of course, further investigations are needed before the new technology can be used on a regular basis.
Keywords: 3D printing, traditional thermoplastic, head film, cranial radiotherapy, CBCT

 Global reach, higher impact
Global reach, higher impact