Impact Factor
ISSN: 1837-9664
J Cancer 2023; 14(11):2145-2151. doi:10.7150/jca.85939 This issue Cite
Research Paper
Surgical results and quality of life after single-stage posterior transpedicular approach for circumferential epidural decompression in patients with thoracolumbar spine metastasis
Musculoskeletal Tumor Centre, Peking University People's Hospital, 11# Xizhimen South Road, Xicheng District, Beijing, China, 100044.
* These authors contributed equally to this study.
Received 2023-5-8; Accepted 2023-7-2; Published 2023-7-9
Abstract
Objective: The primary aim of this study was to evaluate the effect of palliative surgery using posterior transpedicular approach (PTA) with posterior instrumentation on pain response and quality of life (QoL) in patients with metastatic thoracic and lumbar tumors.
Methods: From 2018 to 2019, 39 patients with metastatic thoracic and/or lumbar tumors were prospectively enrolled to measure the reduction in pain and the changes in QoL after surgical decompression with posterior instrumentation via PTA. The patient group was composed of 27 men and 12 women with a mean age of 60 years (range, 28 to 92 years). Pain response was measured using the visual analog scale (VAS) and neurologic status was evaluated using Frankel grades. QoL was assessed with use of the EORCT QLQ-BM22 questionnaire before surgery (baseline) and at 1-, 3-, 6-, and 12-month after surgery. The survival times of all the patients were also collected.
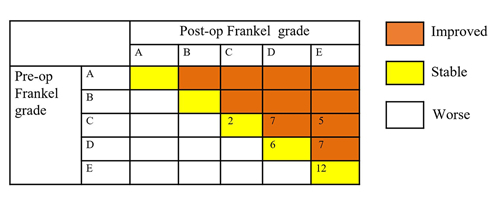
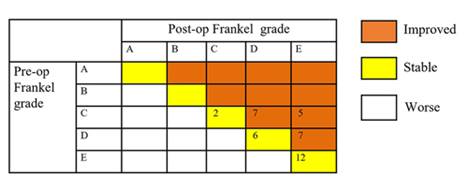
Results: All patients showed either an improvement or a similar pain level after surgery, which the VAS score decreased from 7.10 ± 2.22 preoperatively to 3.10 ± 2.15 one month postoperatively (P<0.05). 19 patients (48.7%, 19/39) showed neurological function improvement postoperatively. Among the 19 patients, 7 cases improved from Frankel grade C to D, 5 cases from grade C to E, and 7 cases from grade D to E. Another 20 patients still have the same Frankel grade postoperatively, however, most of them improved clinically. The QoL improvement of the patients was also evident after treatment. Paired-samples T-test examination of the postoperative scores showed a significant improvement in terms of pain location, pain severity and performance status (P<0.01). Compared with the preoperative score, the 1-month postoperative score of functional interference was significantly improved (63.6 vs. 34.5, P<0.01). There were no significant changes in social or psychological functioning. Three patients experienced cerebrospinal fluid leakage postoperatively, and they were all successfully managed by lying flat without a pillow. One patient experienced rod breakage, at 10 months after surgery. All the patients were alive at 3 months; however, 7 patients died within 3 to 6 months, and another 9 patients died from the disease within 6 to 12 months.
Conclusions: The present feasibility study found that the application of the PTA for decompression and fusion in patients with spinal metastases is beneficial for achieving prompt and sustained pain relief, reducing neurologic deficits and improving functional outcomes, health utilities, and HRQoL.
Keywords: spinal metastases, surgery, quality of life
Introduction
The spine is the most common boney location for cancer metastases [1, 2]. Approximately, spinal metastases presents in 30% to 40% of patients with malignant tumor[3, 4], and it is expected that a group of these patients have symptomatic metastatic lesions of the spinal column. Epidural compression caused by mechanical instability will happen in 5% to 20% of patients, which leading to clinical symptoms, such as neurological dysfunction and intractable pain[3]. These symptoms can gradually result in severe deterioration in the patients' quality of life (QoL) [2, 5, 6]. Therapeutic options for metastatic lesions in spine include radiotherapy, external irradiation, minimally surgery, or open surgery. In certain circumstances, for those with intractable pain, worsening neurological function, or instabilities of spine, radioiodine, and external irradiation may not produce quick outcomes. Therefore, surgical treatment should be taken into consideration if the patient has a good general state. Minimally invasive procedures including vertebroplasty and kyphoplasty can be performed to achieve pain relief and restore some degree of stability, however, they do not allow for the tumor resection and resolve the epidural compression.
Overall, those with metastatic spinal tumors are usually older, and have diminished pulmonary function and general state. Consequently, the anterior approach is not recommended for these patients[7]. To decrease the morbidity encountered in the combined anterior-posterior surgical procedure, circumferential decompression with a single posterolateral transpedicular approach (PTA) can be performed[8-10]. Surgery for spinal metastases is a palliative option, and the goals of treatment are to improve and maintain patients' activity of daily living and QoL until the end-state. Patient reported outcome (PRO) measures are important for analyzing the effect of disease and therapy on patient symptoms [11]. Therefore, this prospective study aim to use validated PRO measurements and pain outcomes to assess the efficacy of single-stage PTA for circumferential epidural decompression and posterior instrumentation.
Materials and Methods
This prospective clinical study was approved by the Ethical Review Committee of Peking University People's Hospital (No. 2020PHB149-01). Patients were prospectively enrolled from January 2018 to December 2019. The inclusion criteria were as follows: (i) patients who were over 18 years with a sober consciousness and has the ability to understand and fill in the questionnaires; (ii) patients with thoracolumbar vertebral metastases suffered severe pain, pathologic fractures and metastatic epidural spinal cord compression (MESCC). Patients with radio-resistant or previously radiated spinal lesions were also included in our study. Patients who could not tolerate operation or who had a predicted survival time less than 3 months were excluded. The predicted survival time of patients with spinal metastases was evaluated according to the revised Tokuhashi scoring system[12].
Quality of Life Assessment
The European Organization for Research and Treatment of Cancer Quality of Life Questionnaire for Patients with Bone Metastases (EORTC QLQ-BM22) is used to assess disease symptoms related to bone metastases[13, 14]. As a PRO measure for patients with bone metastases, it has been translated to Chinese version and has been validated in Chinese population for measuring QoL[15]. The questionnaire comprises 22 items and 4 scales for the measurement of pain in different parts of the body (painful sites), pain characteristics (persistent pain, recurrent pain), functional impairment (occurrence of pain when performing different activities, interference with everyday activities), and psychosocial aspects (family, worries, hope). All items were graded from 1 point (not at all) to 4 point (very much). A higher grade indicates greater distress in symptom scales while a higher grade in functional scale indicates greater functional outcome. Each grade was converted to a score ranging from 0 to 100.
Surgical Technique
General anesthesia was performed in each patient. Then the patient was placed in the prone position, a midline incision was performed extending over the two lower and two upper vertebral over the lesion level. Exposure of posterior portions of the vertebra was made. Intraoperative C-arm visualization was used to detect the accurate vertebral level.
Initially, transpedicular screws were placed into the two vertebrae upper and lower the damaged vertebra. A rongeur was used to remove the posterior spinous processes. Subsequently, laminectomy was performed by laminectomy rongeur. A temporary rod can be placed on one side after the removal of the posterior complex, which provides temporary stabilization against the instability caused by posterior complex decompression and protect nerve tissues from damage caused by unintended vibrations during manipulation.
Bilateral laminectomy, facetectomy, and wide foraminotomy were performed on the lower and upper levels of the damaged vertebra. The intervertebral disc spaces of the damaged vertebra were emptied and 360 degree debridement was performed either directly via the tissue mass or via the spaces between the nerve roots with a transpedicular approach.
After complete decompression of the neural structures and removal of the tumor, vertebral cement augmentation was performed to reconstruct the anterior column of the spine. Finally, the screws above and below the involved vertebral segment and the rod were fixed, and the system was stabilized posteriorly.
Follow-up and Data Collection
The Chinese-language version of the EORTC QLQ-BM22 questionnaire was administered at baseline (before surgery) and at one, three, six, and twelve months postoperativelly. The patients received and returned the questions by a questionnaire software or paper version. Moreover, the Karnofsky performance score was used to present the general condition of patients. The visual analog scale (VAS) was used to evaluate pain, and Frankel grade was utilized to assess neurological function.
Statistical Analyses
Statistical analyses were carried out by using SPSS software, version 22.0 (Armonk, NY, USA). Normally distributed data were recorded using the means ± standard deviation (SD), while nonnormally distributed data were presented as the medians and range. Paired t-tests were used to compare the scores of each scale of the EORTC QLQ-BM22 at one, three, six, and twelve months with the baseline score. Preoperative and postoperative VAS scores were compared by using paired t-test. Kaplan-Meier curves were obtained, the date of surgery was the starting date, and death or the last known contact date was the censor date. A P value < 0.05 was considered significant, and a power analysis was conducted.
Results
Preoperative Demographic Data
There were 27 male and 12 female with an average age at the time of surgery of 60 years (SD, 14; range, 28 to 92 years). The most common origin of the primary tumor was the liver in 20.5%, followed by the lung, breast and kidney in 15.4% of cases each (Table 1). Two cases had MESCC from an unknown primary site of origin. The median time from the diagnosis of the primary cancer to spinal metastasis was 32 months (SD, 77; range, 0 to 480 months). Twelve patients had multimetastatic disease to visceral organs at the time of surgery. The average Karnofsky performance score was 47, ranging from 20 to 90.
Surgical Data
All patients underwent planned surgeries and there was no intraoperative death. The mean operative duration was 243 minutes (range, 130 to 450 minutes). The mean intraoperative blood loss was 1417 mL (range, 200 to 3500 mL). No notable intraoperative complications were observed. Three patients experienced cerebrospinal fluid leakage postoperatively, and they were all successfully managed by lying flat without a pillow. One patient experienced rod breakage at 10 months after surgery who received a revison surgery.
Postoperative Outcomes
All patients showed either an improvement or a similar pain level after surgery (Table 2). The VAS score decreased from 7.10 ± 2.22 preoperatively to 3.10 ± 2.15 one month postoperatively (P<0.05). As shown in Figure 1, The Frankel grades decreased significantly after operation. Among 39 patients, preoperatively, 3 were evaluated as Frankel grade B, 5 as Frankel grade C, 11 as Frankel grade D, and 2 as Frankel grade E. Postoperatively, 19 patients (48.7%, 19/39) showed neurological function improvement. Among the 19 patients, 7 cases improved from Frankel grade C to D, 5 cases from grade C to E, and 7 cases from grade D to E. Another 20 patients still have the same Frankel grade postoperatively, however, most of them improved clinically.
The QoL improvement of the patients was also evident after treatment. The EORTC QLQ-BM22 scores of the patients before treatment and 1-month (39 cases), 3-months (39 cases), 6-months (32 cases), and 12-months (23 cases) after treatment are shown in Table 3. Paired-samples T-test examination of the postoperative scores showed a significant improvement in terms of pain location, pain severity and performance status (P<0.01). The painful sites scores were 14.5 (SD, 12.4), 13.5 (SD, 12.9), 11.9 (SD, 13.1) and 11.0 (SD, 10.8) at the 1-, 3-, 6-, and 12-months after surgery, respectively. Additionally, painful characteristics were more pronounced in this group of patients, which were 26.5, 25.6, 18.1 and 16.4 at 1-, 3-, 6-, and 12-months after treatment, respectively, compared to 53.0 preoperatively. With regard to functional interference, there was significant improvement one month postoperatively compared with the preoperative score (63.6 vs. 34.5, P<0.01). As shown in Table 3, there were no significant changes in social or psychological functioning.
Survival
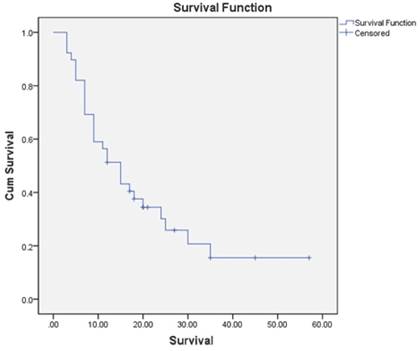
The mean follow-up was 15.9 months (SD, 12 months; range, 3 to 57 months). All the patients were alive at 3 months; at 3 to 6 months 7 patients were dead, and at 6 to 12 months, another 9 patients died of disease. During follow-up, 29 patients died. The K-M survival estimate at 1 year postoperatively was 51.3%, and that at 2 years was 30.2% (Figure 2).
Demographic Data of the Patients
| No. | Sex | Age | Tumor level | Tumor Pathology | Interval time | Visceral metastasis | KPS |
|---|---|---|---|---|---|---|---|
| 1 | F | 65 | L3 | Lung | 0 | 60 | |
| 2 | M | 47 | L5 | Liver cancer | 0 | 60 | |
| 3 | M | 66 | L3 | Unknown | 36 | 40 | |
| 4 | M | 49 | L3 | Lung | 0 | 50 | |
| 5 | F | 66 | L4 | Renal carcinoma | 24 | 50 | |
| 6 | M | 69 | L3 | Renal carcinoma | 36 | 40 | |
| 7 | M | 82 | T4 | Prostate carcinoma | 2 | 40 | |
| 8 | M | 78 | T11 | Liver cancer | 23 | Liver | 50 |
| 9 | F | 46 | T5, T6 | Breast carcinoma | 72 | 70 | |
| 10 | F | 63 | L3 | Thyroid carcinoma | 84 | Lung | 50 |
| 11 | F | 53 | L1 | Breast carcinoma | 56 | 60 | |
| 12 | M | 61 | T5, T6, | Urothelial carcinoma | 24 | Liver | 30 |
| 13 | F | 68 | T2 | Breast carcinoma | 0 | 30 | |
| 14 | F | 72 | T8, T9 | Breast carcinoma | 18 | 50 | |
| 15 | M | 69 | T3 | Renal carcinoma | 36 | 40 | |
| 16 | M | 64 | T6 | Rectal | 0 | 30 | |
| 17 | M | 60 | T2 | Rectal | 22 | Liver | 40 |
| 18 | F | 43 | T4 | Breast carcinoma | 16 | 30 | |
| 19 | M | 60 | L4 | Lung | 12 | Liver | 50 |
| 20 | M | 60 | L3 | Rectal | 64 | Lung | 90 |
| 21 | M | 59 | T9 | Renal carcinoma | 84 | Lung\brain | 80 |
| 22 | M | 70 | T12 | Liver cancer | 6 | 50 | |
| 23 | F | 72 | L4 | Leiomyosarcoma of uterus | 48 | Lung | 40 |
| 24 | M | 36 | L1 | Liver cancer | 3 | Liver | 80 |
| 25 | M | 67 | T12 | Liver cancer | 12 | 50 | |
| 26 | M | 28 | T4、T5 | Lung | 0 | 50 | |
| 27 | M | 56 | L2 | Thyroid carcinoma | 0 | 50 | |
| 28 | M | 58 | T3 | Renal carcinoma | 24 | 70 | |
| 29 | F | 49 | L1 | Cervical cancer | 35 | 40 | |
| 30 | M | 49 | T12 | Liver cancer | 9 | 50 | |
| 31 | M | 70 | L2 | Unknown | 0 | 40 | |
| 32 | F | 58 | T9, T11 | Myeloma | 0 | 20 | |
| 33 | M | 92 | T4 | Renal carcinoma | 7 | 40 | |
| 34 | M | 33 | T5, T12 | Liver cancer | 0 | 30 | |
| 35 | M | 56 | T6 | Rectal | 6 | 40 | |
| 36 | F | 71 | T3 | Breast carcinoma | 480 | 50 | |
| 37 | M | 82 | L3 | Lung | 0 | Liver | 30 |
| 38 | M | 57 | T11 | Lung | 0 | Mediastinum | 50 |
| 39 | M | 39 | T6 | Liver cancer | 21 | Liver | 30 |
M: Male; F: Female
Changes in pre- and postoperative Frankel grades.
Discussion
The incidence of metastatic spine tumors has increased considerably as a result of the technological development of early diagnosis methods[16]. The expected survival time of those with malignant tumors also been prolonged in recent decades. Decompression and stabilization are indicated in patients with spinal metastases or nonpathological fractures who have high-grade epidural compression with or without neurological deficits and three-column instability. Since most treatment for bone metastasis are palliative in nature, health-related QoL (HRQoL) is theoretically a more meaningful end point together with symptom control, when compared with traditional end points such as survival times and local control [17]. HRQoL focused on the patient's feelings and experience after treatment. HRQoL issues are of critical importance for patients, when making decisions in the treatment of bone metastases. To date, there are few prospective studies on surgical outcomes and changes in QoL after surgery in patients with spinal metastases [5, 18, 19]. Therefore, we conducted this prospective study to investigate the change in HRQoL in a consecutive series of patients who underwent palliative surgery for vertebral metastases.
Kaplan-Meier overall survival curve of 39 patients.
The surgical outcome of all patients
| No. | Pre-op VAS | Post-op VAS | Pre-op Frankel | Post-op Frankel | Followup Time (month) | End |
|---|---|---|---|---|---|---|
| 1 | 6 | 2 | E | E | 7 | DOD |
| 2 | 7 | 3 | E | E | 35 | DOD |
| 3 | 7 | 3 | C | D | 57 | AWD |
| 4 | 8 | 8 | D | D | 7 | DOD |
| 5 | 7 | 4 | D | D | 18 | DOD |
| 6 | 8 | 1 | C | D | 7 | DOD |
| 7 | 1 | 0 | C | D | 35 | AWD |
| 8 | 7 | 1 | D | E | 17 | DOD |
| 9 | 7 | 3 | E | E | 15 | DOD |
| 10 | 7 | 6 | D | D | 25 | DOD |
| 11 | 7 | 5 | D | E | 45 | AWD |
| 12 | 7 | 5 | D | E | 11 | DOD |
| 13 | 8 | 4 | C | D | 12 | NED |
| 14 | 8 | 3 | E | E | 15 | DOD |
| 15 | 8 | 1 | C | E | 5 | DOD |
| 16 | 8 | 2 | C | E | 27 | AWD |
| 17 | 10 | 3 | D | D | 5 | DOD |
| 18 | 5 | 2 | D | E | 30 | DOD |
| 19 | 7 | 2 | E | E | 9 | DOD |
| 20 | 3 | 1 | E | E | 24 | DOD |
| 21 | 2 | 1 | E | E | 20 | DOD |
| 22 | 9 | 2 | D | E | 12 | DOD |
| 23 | 10 | 7 | D | D | 15 | DOD |
| 24 | 7 | 5 | E | E | 4 | DOD |
| 25 | 7 | 3 | D | E | 3 | DOD |
| 26 | 9 | 6 | E | E | 9 | DOD |
| 27 | 7 | 0 | C | E | 18 | AWD |
| 28 | 5 | 2 | E | E | 5 | DOD |
| 29 | 10 | 6 | C | D | 12 | DOD |
| 30 | 7 | 3 | E | E | 3 | DOD |
| 31 | 9 | 6 | C | C | 3 | DOD |
| 32 | 7 | 4 | C | D | 17 | AWD |
| 33 | 1 | 0 | C | D | 20 | AWD |
| 34 | 8 | 2 | C | E | 9 | DOD |
| 35 | 8 | 7 | C | C | 7 | DOD |
| 36 | 10 | 1 | D | E | 20 | AWD |
| 37 | 10 | 0 | D | D | 21 | AWD |
| 38 | 7 | 4 | E | E | 9 | DOD |
| 39 | 8 | 3 | C | E | 7 | DOD |
DOD: Died of disease; AWD: Alive with disease; NED: No evidence of disease
Patients' health-related quality of life evaluation by EORTC QLQ-BM22
| Scale | Before surgery | Follow-up at 1 months (N=39) | Follow-up at 3 months (N=39) | Follow-up at 6 months (N=32) | Follow-up at 12 months (N=23) |
|---|---|---|---|---|---|
| Painful sites | 33.8±20.3 | 14.5±12.4* | 13.5±12.9* | 11.9±13.1* | 11.0±10.8* |
| Painful characteristics | 53.0±29.2 | 26.5±23.6* | 25.6±25.8* | 18.1±18.5* | 16.4±16.0* |
| Functional interference | 34.5±28.3 | 63.6±24.1* | 67.6±21.7* | 71.2±20.1* | 69.9±17.9* |
| Psychosocial aspects | 56.4±21.8 | 53.3±16.6 | 54.0±16.3 | 49.3±17.3 | 47.6±16.4 |
* P<0.05 compared with the scores before surgery
Compared with radiotherapy, external irradiation, or minimally invasive procedures such as vertebroplasty or kyphoplasty, open surgery has the conceptual benefit of providing direct spinal cord decompression, reduction of local tumor burden, and the opportunity for mechanical stabilization of the diseased spine. In addition, surgical decompression provides cytoreduction and a margin around neural elements, that is, separation surgery, allowing subsequent adjuvant therapy, which is associated with improved local tumor control[20-23].
The various surgical approaches used to treat spinal metastasis include the following: anterior transcavitary and posterior, posterolateral (transpedicular, costotransversectomy, lateral extracavitary), and a combined approach. Because tumor location, the type of reconstruction needed, patient comorbidities, the extent of primary tumor, and the surgeon's preference have a great impact on the surgical approach, it is essential that the best surgical approach from the patient's perspective be carefully considered before surgery. In the past, many published retrospective studies have shown that 360 degree decompression with a single PTA provides circumferential decompression and stabilization simultaneously, which is associated with less morbidity in systemically compromised patients[10, 24]. The present study, based on 39 consecutive patients enrolled with spinal metastases, shows that 360 degree decompression with a single PTA results in significant improvements in pain, neurological function and HRQoL.
Patient-reported HRQoL outcome measures convey information that can be critical in clinical decision making. Among other HRQoL-measuring instruments, the EORTC QLQ-BM22 can effectively detect changes in QoL in diverse bone metastasis populations. This study shows that decompression with a single PTA improves pain, neurologic and functional status, and that EORTC QLQ-BM22 can measure health utilities and HRQoL for symptomatic patients. Compared with preoperative scores, postoperative EORTC QLQ-BM22 scores for painful sites, pain characteristics, and functional interference scale were significantly lower at the 1-month and 3-, 6-, and 12-month follow-ups. As investigators mention in several other studies, spinal surgery for MESCC is associated with rapid, substantial, and sustained pain relief[5, 18]. Healthcare professionals will be able to reliably assess their patients' QoL, help patients choose a treatment and assess the cost-effectiveness of the treatments. QoL outcomes in patients with bone matastasis will be compared across clinical trials through the utilization of a consistent and valid questionnaire.
In a previous study, researchers reported that the Eastern Cooperative Oncology Group (ECOG), the Short Form 36 Health Survey (SF-36), the VAS scale, and the assessment of ambulatory status and motor function effectively evaluated the factors that influence the health status of patients with spinal neoplastic disease. In a retrospective study, Chen et al. [25] reported that the EORTC QLQ-BM22 questionnaire showed improved QoL outcomes in patients with spinal metastasis after microinvasive surgery combined with intraoperative radiotherapy. Our results support the fact that surgery improves function and QoL outcomes in patients with metastatic thoracic and lumbar tumors.
In this study, the psychosocial aspects in the EORTC QLQ-BM22 did not reach statistical significance after surgery; which is predominantly due to the small sample size. In addition, patients had different concerns. For example, some patients worried less about a potential loss of mobility, and more about economic factors. Some patients were more worried about becoming dependent on others. Moreover, patients with MESCC represent a frail population with few reserves to deal with additional physical or emotional stress. In future studies, more cases should be included so that each psychosocial items for each individual question can be analyzed to identify areas in which differences are particularly apparent.
This study has several limitations. Although this is a prospective single center study, it is limited by its small sample size and lack of controls. Second, there is no stratification by pathological type due to the small sample of patients. Prospective clinical studies are necessary to further investigate the long-term treatment outcomes of surgery for spinal metastases.
Nonetheless, the present feasibility study found that the application of the posterolateral transpedicular approach for decompression and fusion in patients with spinal metastases can also benefit patients with MESCC in that it achieves prompt and sustained pain relief, reduceds neurolofic deficits and improves functional outcomes, health utilities and HRQoL. Given the overall low incidence, clinical heterogeneity, and rapid development of more efficient medical therapies for the treatment of MESCC, we support current efforts to collect prospective longitudinal data on spine oncology patients.
Abbreviations
PTA: Posterior transpedicular approach; QoL: Quality of Life; PRO: Patient reported outcome; MESCC: Metastatic epidural spinal cord compression; EORTC QLQ-BM22: The European Organization for Research and Treatment of Cancer Quality of Life Questionnaire for Patients with Bone Metastases; VAS: Visual analog scale; SD: Standard deviation; HRQoL: Health-related QoL; ECOG: Eastern Cooperative Oncology Group; SF-36: Short Form 36 Health Survey.
Author contributions
JFN: Designing the study, Collecting and analyzing the data, Preparing the manuscript.
ZQZ: Designing the study, Collecting and analyzing the data, Preparing the manuscript.
JCW: Collecting and analyzing the data, Preparing the manuscript.
TQY: Designing the study, Analyzing the data, Preparing the manuscript, Supervision.
WG: Collecting the data, Preparing the manuscript.
RLY: Collecting the data, Preparing the manuscript.
XDT: Collecting the data, Preparing the manuscript.
Competing Interests
The authors have declared that no competing interest exists.
References
1. Cole JS, Patchell RA. Metastatic epidural spinal cord compression. The Lancet Neurology. 2008;7:459-66
2. Prasad D, Schiff D. Malignant spinal-cord compression. The Lancet Oncology. 2005;6:15-24
3. Klimo P Jr, Schmidt MH. Surgical management of spinal metastases. The oncologist. 2004;9:188-96
4. Wong DA, Fornasier VL, MacNab I. Spinal metastases: the obvious, the occult, and the impostors. Spine. 1990;15:1-4
5. Fehlings MG, Nater A, Tetreault L, Kopjar B, Arnold P, Dekutoski M. et al. Survival and Clinical Outcomes in Surgically Treated Patients With Metastatic Epidural Spinal Cord Compression: Results of the Prospective Multicenter AOSpine Study. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2016;34:268-76
6. Chow E, Bottomley A. Understanding the EORTC QLQ-BM22, the module for patients with bone metastases. Expert review of pharmacoeconomics & outcomes research. 2009;9:461-5
7. Miscusi M, Polli FM, Forcato S, Ricciardi L, Frati A, Cimatti M. et al. Comparison of minimally invasive surgery with standard open surgery for vertebral thoracic metastases causing acute myelopathy in patients with short- or mid-term life expectancy: surgical technique and early clinical results. Journal of neurosurgery Spine. 2015;22:518-25
8. Akeyson EW, McCutcheon IE. Single-stage posterior vertebrectomy and replacement combined with posterior instrumentation for spinal metastasis. Journal of neurosurgery. 1996;85:211-20
9. Bilsky MH, Boland P, Lis E, Raizer JJ, Healey JH. Single-stage posterolateral transpedicle approach for spondylectomy, epidural decompression, and circumferential fusion of spinal metastases. Spine. 2000;25:2240-9 discussion 250
10. Gezercan Y, Çavuş G, Ökten AI, Menekşe G, Çıkılı M, Adamhasan F. et al. Single-Stage Posterolateral Transpedicular Approach With 360-Degree Stabilization and Vertebrectomy in Primary and Metastatic Tumors of the Spine. World neurosurgery. 2016;95:214-21
11. Lipscomb J, Gotay CC, Snyder CF. Patient-reported outcomes in cancer: a review of recent research and policy initiatives. CA: a cancer journal for clinicians. 2007;57:278-300
12. Tokuhashi Y, Matsuzaki H, Oda H, Oshima M, Ryu J. A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine. 2005;30:2186-91
13. Chow E, Hird A, Velikova G, Johnson C, Dewolf L, Bezjak A. et al. The European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire for patients with bone metastases: the EORTC QLQ-BM22. European journal of cancer (Oxford, England: 1990). 2009;45:1146-52
14. Chow E, Nguyen J, Zhang L, Tseng LM, Hou MF, Fairchild A. et al. International field testing of the reliability and validity of the EORTC QLQ-BM22 module to assess health-related quality of life in patients with bone metastases. Cancer. 2012;118:1457-65
15. Zhang L, Su YJ, Chen JY, Liao ZC, Luo ZQ, Xie SM. et al. Validation of the Chinese version of EORTC QLQ-BM22 in patients with bone metastases. Supportive care in cancer: official journal of the Multinational Association of Supportive Care in Cancer. 2016;24:1019-24
16. Wang J, Ni XZ, Yang ML, Huang X, Hou SM, Peng C. et al. Prognostic factors and treatment outcomes of spinal osteosarcoma: Surveillance, epidemiology, and end results database analysis. Front Oncol. 2023;13:1083776
17. Tang Y, Qu J, Wu J, Liu H, Chu T, Xiao J. et al. Effect of Surgery on Quality of Life of Patients with Spinal Metastasis from Non-Small-Cell Lung Cancer. The Journal of bone and joint surgery American volume. 2016;98:396-402
18. Quan GM, Vital JM, Aurouer N, Obeid I, Palussière J, Diallo A. et al. Surgery improves pain, function and quality of life in patients with spinal metastases: a prospective study on 118 patients. European spine journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2011;20:1970-8
19. Barzilai O, McLaughlin L, Amato MK, Reiner AS, Ogilvie SQ, Lis E. et al. Predictors of quality of life improvement after surgery for metastatic tumors of the spine: prospective cohort study. The spine journal: official journal of the North American Spine Society. 2018;18:1109-15
20. Laufer I, Iorgulescu JB, Chapman T, Lis E, Shi W, Zhang Z. et al. Local disease control for spinal metastases following "separation surgery" and adjuvant hypofractionated or high-dose single-fraction stereotactic radiosurgery: outcome analysis in 186 patients. Journal of neurosurgery Spine. 2013;18:207-14
21. Moussazadeh N, Laufer I, Yamada Y, Bilsky MH. Separation surgery for spinal metastases: effect of spinal radiosurgery on surgical treatment goals. Cancer control: journal of the Moffitt Cancer Center. 2014;21:168-74
22. Al-Omair A, Masucci L, Masson-Cote L, Campbell M, Atenafu EG, Parent A. et al. Surgical resection of epidural disease improves local control following postoperative spine stereotactic body radiotherapy. Neuro-oncology. 2013;15:1413-9
23. Bate BG, Khan NR, Kimball BY, Gabrick K, Weaver J. Stereotactic radiosurgery for spinal metastases with or without separation surgery. Journal of neurosurgery Spine. 2015;22:409-15
24. Cho DC, Sung JK. Palliative surgery for metastatic thoracic and lumbar tumors using posterolateral transpedicular approach with posterior instrumentation. Surgical neurology. 2009;71:424-33
25. Chen K, Huang L, Cai Z, Shi J, You K, Shen H. Micro-invasive surgery combined with intraoperative radiotherapy for the treatment of spinal metastasis. European spine journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2017;26:1893-901
Author contact
![]() Corresponding author: Taiqiang Yan, Musculoskeletal Tumor Center, Peking University People's Hospital, Beijing, China. Phone numbers: +86 13910733583; Email: yantqzhcom.
Corresponding author: Taiqiang Yan, Musculoskeletal Tumor Center, Peking University People's Hospital, Beijing, China. Phone numbers: +86 13910733583; Email: yantqzhcom.

 Global reach, higher impact
Global reach, higher impact