3.2
Impact Factor
ISSN: 1837-9664
J Cancer 2016; 7(9):1169-1173. doi:10.7150/jca.15037 This issue Cite
Research Paper
Body Mass Index Is Positively Associated with Endometrial Cancer in Chinese Women, Especially Prior to Menopause
1. The Hospital of Obstetrics & Gynaecology, Fudan University, China
2. Section of Epidemiology and Biostatistics, School of Population Health, The University of Auckland, New Zealand
3. Department of Obstetrics & Gynaecology, The University of Auckland, New Zealand
Received 2016-1-20; Accepted 2016-4-26; Published 2016-6-6
Abstract
Objective: Obesity is a well-known risk factor for developing endometrial cancer. However, the incidence and survival rate of endometrial cancer are associated with ethnicity and geographical area. In addition, whether menopausal status is associated with developing endometrial cancer in obese women and whether obesity is associated with subtypes of endometrial cancer have not been fully investigated. Here, we investigated the effect of BMI on developing endometrial cancer in Chinese women taking into account menopausal status and cancer subtypes.
Methods: Data on 1,127 women with endometrial cancer including body mass index (BMI), age at diagnosis, parity, menopausal status and cancer subtype were collected from the largest obstetrics & gynaecology hospital in China and analysed.
Results: After adjusting for age and parity, the odds for developing endometrial cancer in overweight or obese perimenopausal women was significantly higher than that in women with normal weight (OR=2.6 with 95%CI:1.9-3.5, and OR=3.5 with 95%CI: 2.2-5.4, respectively). The odds of developing endometrial cancer in overweight postmenopausal women were significantly higher than that in women who were normal weight (OR=2.4 with 95%CI: 1.8-3.1), however this was not the case for obese postmenopausal women. We further found that BMI, menopausal status, age and parity were not associated with subtypes of endometrial cancer.
Conclusion: Our data demonstrate that obesity is positively associated with the incidence of developing endometrial cancer in Chinese women, with more significant effects in perimenopausal women.
Keywords: BMI, endometrial cancer, menopause, type I and type II, Chinese women
Introduction
Endometrial cancer is the most common cancer of the female reproductive tract in developed countries and is the third most common cause of death from female cancers. In 2012, it occurred in 320,000 women and caused 76,000 deaths worldwide [1]. The number of endometrial cancer has rapidly increased in Chinese women over the last ten years [2].The exact cause of endometrial cancer remains unknown, although several risk factors have been identified, including early menarche, nulliparity, late menopause, diabetes mellitus, hypertension, obesity, ethnicity and family history of endometrial cancer [3-8].
Obesity, as measured by body mass index, is a well-known risk factor for developing endometrial cancer. Recent meta-analyses suggest that women who are overweight or obese have a 1.43 or 3.33 fold increase in risk for developing endometrial cancer, respectively, compared to women with normal weight [9]. However, a number of studies have reported that the incidence and survival rate of endometrial cancer are associated with ethnicity and geographical area [10-12]. Indeed, Chinese women will have different lifestyle and dietary habits compared to European or American women. The World Health Organisation (WHO) classification of BMI for Asians is also different from that for Caucasians. The WHO ethnic-specific BMI distribution data show that 10-12% of Chinese women are underweight (BMI<18.4), around 70% are normal weight (BMI=18.5-22.9 kg/m2), 10-15% are overweight (BMI=23-27.49 kg/m2), and only 2-3% are obese (BMI>27.50 kg/m2) [13].
Most women with endometrial cancer in developed countries are diagnosed between the ages of 60 and 70 years old, and the average age is 61 [14]. However, for the Chinese population, the mean age at diagnosis of endometrial cancer is younger (57 years old) than Caucasian women (64 years old) [12]. A recent study also showed that 38.1% of Chinese women with endometrial cancer were diagnosed before menopause, compared to less than 25% of Caucasian women [2]. Studies have reported that overweight/obesity is associated with the development of endometrial cancer in Chinese women [15-18]. One of these studies suggested that the association between cancer and obesity are relatively small in Chinese population [18], other study suggested that weight gain before menopause has significantly effect on development of endometrial cancer [17]. However, some of these studies used the WHO classification of BMI for Europeans and Americans, not for Asians. In addition, none of these studies take into account menopausal status and subtypes of endometrial cancer to associate with BMI.
Endometrial cancer is commonly divided into type I and type II, based on clinical features and pathogenesis. The two subtypes are also genetically distinct [19]. Type I endometrial cancer is estrogen dependent and represent 75-90% of endometrial cancer [19], while type II endometrial cancer is estrogen independent. To date there are no previous studies investigating the relationship between obesity and type I and type II endometrial cancer.
Therefore, we undertook this study to investigate the effect of BMI on the risk of developing endometrial cancer in Chinese women, taking into account menopausal status and cancer subtype.
Materials and Methods
This study was approved by the Ethics Committee of The Hospital of Obstetrics & Gynaecology, Fudan University, China.
Study participants
The retrospective data in this case control study were collected from January 2011 to December 2014 from The Hospital of Obstetrics and Gynaecology, Fudan University. This is the largest Obstetrics & Gynaecology university teaching hospital, serving a diverse urban and rural population in Shanghai, the largest city in China with a population of 20 million. Data on all patients admitted to the hospital with a primary diagnosis of endometrial cancer were collected according to the electronic based medical records of patients. Clinical characteristics included age at diagnosis, self-reported age at menopause, and parity. Patients were matched one to one by age frequency with women who underwent routine health examination were randomly selected from the same hospital during the same time period.
Body mass index (BMI) was measured and calculated as the ratio of maternal weight and height (kg/m2) at diagnosis. According to the WHO classification of BMI for Asian/Indian women, the BMIs for underweight, normal weight, overweight and obese are under 18.4 kg/m2, 18.5-22.99 kg/m2, 23-27.49 kg/m2 and over 27.50 kg/m2, respectively.
Statistical analysis
The effect of BMI, menopause and the interaction between BMI and menopause on the incidence of endometrial cancer adjusting for age and parity was analysed by logistic regression method using SAS software version 9.3 (SAS Institute Inc., Cary, NC, USA) with p <0.05 being considered statistically significant.
Clinical characteristics of women with endometrial cancer
| Endometrial cancer (N=1,127) | Control (n=1,244) | |
|---|---|---|
| Age at diagnosis (years old, median/range) | 55 (26 - 88) | 54 (22-87) |
| Parity (number, %) | ||
| 0 | 94 (8.3%) | 96 (7.7%) |
| 1 | 636 (56.5%) | 878 (70.6%) |
| 2 | 246 (21.8%) | 216 (17.4%) |
| ≥3 | 151 (13.4%) | 54 (4.3%) |
| Menopause | ||
| Perimenopause (number, %) | 489 (43.4%) | 818 (65.7%) |
| Postmenopause (number, %) | 638 (56.6%) | 426 (34.3%) |
| Type I | 904 (80.2%) | N/A |
| Type II | 223 (19.8%) | N/A |
Results
Clinical characteristics of the study population
The clinical characteristics of study participants are summarised in Table 1. The median age of patients at diagnosis was 55 (range 21-85) years old. Of the 1,127 patients, 94 (8.3%) were nulliparous, 489 (43.4%) patients were diagnosed before menopause and 739 (65.5%) were overweight or obese. Of 1,127 patients, 904 (80.2%) were diagnosed with type I endometrial cancer.
Overweight/obesity is associated with the incidence of developing endometrial cancer in Chinese perimenopausal and postmenopausal women
The effect of BMI, menopause and the interaction between BMI and menopause on the probability of developing endometrial cancer was analysed using logistic regression, adjusting for parity and age. Join tests shows that the interaction effect of BMI and menopause on the probability of developing endometrial cancer was highly significant (p=0.0001).
The significant interaction between BMI and menopause indicated the effect of BMI on the odds of developing endometrial cancer was not the same between perimenopausal and postmenopausal women. Therefore, further subgroup analyses were conducted on patients before and after menopause separately (Table 2).
Odds ratios (OR) and 95% confidence intervals (CI) for the effect of BMI on developing endometrial cancer from logistic regression adjusting for age and parity, subgroup analyses by before or after menopause
| BMI | Endometrial cancer (n=1,127) | Control (n=1,244) | OR | 95% CI | p-value | |
|---|---|---|---|---|---|---|
| Before Menopause (number, %) | <.0001 | |||||
| Normal weight (Ref) | 186 (38.0%) | 270 (63.4%) | ||||
| Overweight | 211 (43.1%) | 118 (27.7%) | 2.555 | 1.876 | 3.481 | |
| Obese | 92 (18.8%) | 38 (8.9%) | 3.471 | 2.236 | 5.388 | |
| Total | 489 | 426 | ||||
| After menopause (number) | <.0001 | |||||
| Normal weight (Ref) | 202 (31.7%) | 350 (42.8%) | ||||
| Overweight | 302 (47.3%) | 219 (26.8%) | 2.387 | 1.86 | 3.063 | |
| Obese | 134 (21.0%) | 249 (30.4%) | 0.886 | 0.672 | 1.169 | |
| Total | 638 | 818 | ||||
BMI: Body mass index
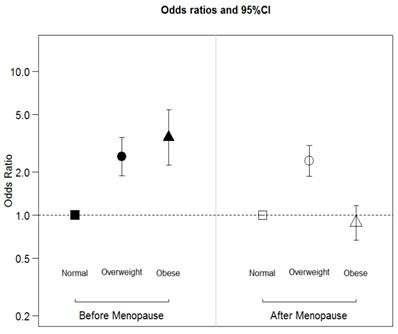
After adjusting for age and parity, the odds for developing endometrial cancer in overweight or obese Chinese perimenopausal women was significantly higher than that in women with normal weight (OR=2.6 with 95%CI:1.9-3.5, and OR=3.5 with 95%CI: 2.2-5.4, respectively) (Figure 1). The odds of developing endometrial cancer in overweight Chinese postmenopausal women were significantly higher than that in women who were normal weight (OR=2.4 with 95%CI: 1.8-3.1). However, there was no significant difference in the risk of developing endometrial cancer in obese Chinese postmenopausal women compared with women who were normal weight (OR=0.886 with 95%CI: 0.67-1.2).
The effect of BMI and menopause in the development of endometrial cancer
BMI, menopause, age and parity are not associated with specific subtypes of endometrial cancer in Chinese women
We further analysed whether BMI, menopausal status, age and parity were associated with subtypes of endometrial cancer (Table 3). None of these risk factors were significantly associated with either subtypes of endometrial cancer.
The distribution of subtypes of endometrial cancer by BMI
| Type I Endometrial cancer (n=904) | Type II Endometrial cancer (n=223) | |||
|---|---|---|---|---|
| Perimenopause (n=413) | Postmenopause (n=491) | Perimenopause (n=76) | Postmenopause (n=147) | |
| Normal weight (n=388) (number, %) | 152 (36.8%) | 154 (31.4%) | 34 (44.7%) | 48 (32.7%) |
| Overweight (n=513) (number, %) | 181(43.8%) | 230 (46.8%) | 30 (39.5%) | 72 (48.9%) |
| Obese (n=226) (number, %) | 80 (19.4%) | 107 (21.8%) | 12 (15.8%) | 27 (18.4%) |
Discussion
The incidence of endometrial cancer varies by ethnicity[10-12], and is increasing in the Chinese population [2]. Obesity is a well-known risk factor for developing endometrial cancer and it has been estimated that 40% of endometrial cancer is associated with obesity [20]. However, few Chinese women are overweight or obese [13]. This stimulated us to investigate whether obesity is a risk factor for developing endometrial cancer specifically in Chinese women.
To date, only one other study has investigated the association between BMI and endometrial cancer in Chinese population [15], which found that women with BMI≥25.0kg/m2were more likely to develop endometrial cancer. In the current study, using WHO BMI classification for Asian women our data show that BMI>23 is associated with the development of endometrial cancer in Chinese women. This result confirms that the general consensus that increased BMI is positively associated with the development of endometrial cancer is also true in the Chinese population.
Interestingly, in the current study we found that there is a significant interaction between BMI and menopause, suggesting that the positive association of BMI and the development of endometrial cancer are dependent on menopausal status. In this study, we found that overweight or obese Chinese perimenopausal women were three times more likely than normal-weight women to develop endometrial cancer. Overweight Chinese postmenopausal women were twice as likely as normal-weight women to develop endometrial cancer. However, there was no significant difference in developing endometrial cancer between Chinese postmenopausal women who were obese and Chinese postmenopausal women with normal weight. We cannot currently explain our finding that obesity is not associated with the risk of developing endometrial cancer in postmenopausal women but this result may suggest that the effects of obesity on the incidences of endometrial cancer are not fully understood [21].
In Western countries, endometrial cancer is predominantly diagnosed at an older age (between 60 and 70 years old). However, compared with Caucasians, the age of diagnosis of endometrial cancer is earlier in Asian women including Chinese women [12]. Our recent study also found that 38% of Chinese women were diagnosed with endometrial cancer before menopause [22]. In this current study, we found that 43.4% of women with endometrial cancer were diagnosed before menopause with a median age of 47 years old. We do not know the exact reason for this difference, but ethnicity-specific changes in the levels of different hormones may play a role [23-25]. In addition, high levels of BMI (overweight and obese) are currently more common among middle age (40-50 years old) women in China compared to later age. Another study suggested that weight gain during adulthood, in particular during the time of perimenopause, is associated with the incidence of endometrial cancer [17]. This may be because obesity is associated with an increased frequency of anovulation, a reduction of progesterone synthesis and endometrial exposure to unopposed estrogen in perimenopausal women [21]. High levels of unopposed estrogen, and an imbalance between estrogen and progesterone levels, are some risk factors for developing endometrial cancer.
To date, the majority of studies have considered endometrial cancer as a single disease, however endometrial cancer can be broadly classified into type I and type II, based on clinical features and histology. It is not clear whether the effect of obesity on the development of endometrial cancer is only associated with estrogen-dependent type I endometrial cancer. The shift in progesterone/estrogen balance by menopause may be associated with type I endometrial cancer. However, in this current study, we found that BMI, menopause, age and parity were not associated with the incidence of neither Type I nor Type II endometrial cancer. This is consistent with previous research, which found that parity, a well-known protective factor for the development of endometrial cancer, is not associated with the incidence of the two subtypes of endometrial cancer [22, 26]. This could be because the two types of endometrial cancer share many common risk factors and potentially suggests that type II endometrial cancer may not be completely estrogen independent [27].
China has a lower incidence of endometrial cancer compared with the United States [8], but it is rapidly increasing [2]. This could be due to industrialisation in China from the 1980s and the introduction of the Western/fast-food diet, resulting in the increase in BMI in Chinese women. Therefore, better understanding of the risk factors and development of endometrial cancer in the Chinese population has become imperative. Future research could investigate the incidence and risk factors for endometrial cancer in Chinese women who have immigrated to other developed countries.
There are some limitations in this study in terms of generalizing the findings to China as a whole. All data were obtained from the largest university teaching hospital in the largest city in China over 4 years, which limited the sample size. The association between obesity and endometrial cancer may vary between regions and socioeconomic levels in China due to the different life style and dietary habits. In addition, case control studies are prone to bias, cohort studies would be ideal.
In conclusion, compared to previous studies, in this case control study we found that obesity is positively associated with the incidence of developing endometrial cancer in Chinese women, with more significant effects in perimenopausal women compared to postmenopausal women. More important, to authors' knowledge, this is the first report that BMI, menopause, age and parity are not associated with the two subtypes of endometrial cancer. Endometrial cancer often occurs after menopause in Caucasian women reported in the literature [28], our study may recommend that an endometrial biopsy be performed when obese Chinese women with abnormal uterine bleeding present, even if they are perimenopausal.
Competing Interests
The authors have declared that no competing interest exists.
References
1. Stewart BW, Wild C. World cancer report. Lyon, France. 2014
2. Li X, Zheng S, Chen S, Qin F, Lau S, Chen Q. Trends in gynaecological cancers in the largest obstetrics and gynaecology hospital in China from 2003 to 2013. Tumour Biol. 2015;36(7):4961-6
3. Setiawan VW, Pike MC, Karageorgi S, Deming SL, Anderson K, Bernstein L. et al. Age at last birth in relation to risk of endometrial cancer: pooled analysis in the epidemiology of endometrial cancer consortium. Am J Epidemiol. 2012;176(4):269-78
4. Nichols HB, Trentham-Dietz A, Hampton JM, Titus-Ernstoff L, Egan KM, Willett WC. et al. From menarche to menopause: trends among US Women born from 1912 to 1969. Am J Epidemiol. 2006;164(10):1003-11
5. Karageorgi S, Hankinson SE, Kraft P, De Vivo I. Reproductive factors and postmenopausal hormone use in relation to endometrial cancer risk in the Nurses' Health Study cohort 1976-2004. Int J Cancer. 2010;126(1):208-16
6. Kaaks R, Lukanova A, Kurzer MS. Obesity, endogenous hormones, and endometrial cancer risk: a synthetic review. Cancer Epidemiol Biomarkers Prev. 2002;11(12):1531-43
7. Jamison PM, Noone AM, Ries LA, Lee NC, Edwards BK. Trends in endometrial cancer incidence by race and histology with a correction for the prevalence of hysterectomy, SEER 1992 to 2008. Cancer Epidemiol Biomarkers Prev. 2013;22(2):233-41
8. Dossus L, Allen N, Kaaks R, Bakken K, Lund E, Tjonneland A. et al. Reproductive risk factors and endometrial cancer: the European Prospective Investigation into Cancer and Nutrition. Int J Cancer. 2010;127(2):442-51
9. Jenabi E, Poorolajal J. The effect of body mass index on endometrial cancer: a meta-analysis. Public health. 2015
10. Schorge JO, Williams JW. Williams gynecology Gynecology. New York: McGraw-Hill Medical. 2012
11. Olson SH, Atoria CL, Cote ML, Cook LS, Rastogi R, Soslow RA. et al. The impact of race and comorbidity on survival in endometrial cancer. Cancer Epidemiol Biomarkers Prev. 2012;21(5):753-60
12. Mahdi H, Schlick CJ, Kowk LL, Moslemi-Kebria M, Michener C. Endometrial cancer in Asian and American Indian/Alaskan Native women: tumor characteristics, treatment and outcome compared to non-Hispanic white women. Gynecol Oncol. 2014;132(2):443-9
13. WHO expert consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157-63
14. Akhmedkhanov A, Zeleniuch-Jacquotte A, Toniolo P. Role of exogenous and endogenous hormones in endometrial cancer: review of the evidence and research perspectives. Ann N Y Acad Sci. 2001;943:296-315
15. Zhang Y, Liu Z, Yu X, Zhang X, Lu S, Chen X. et al. The association between metabolic abnormality and endometrial cancer: a large case-control study in China. Gynecol Oncol. 2010;117(1):41-6
16. Ye S, Wen H, Jiang Z, Wu X. The effect of visceral obesity on clinicopathological features in patients with endometrial cancer: a retrospective analysis of 200 Chinese patients. Bmc Cancer. 2016;16(1):209
17. Xu WH, Xiang YB, Zheng W, Zhang X, Ruan ZX, Cheng JR. et al. Weight history and risk of endometrial cancer among Chinese women. Int J Epidemiol. 2006;35(1):159-66
18. Wang D, Zheng W, Wang SM, Wang JB, Wei WQ, Liang H. et al. Estimation of cancer incidence and mortality attributable to overweight, obesity, and physical inactivity in China. Nutr Cancer. 2012;64(1):48-56
19. Hoffman B, Schorge J, Schaffer J, Halvorson LM, Bradshaw K, Cunningham F. et al. Williams Gynecology: Endometrial Cancer 2nd ed. McGraw-Hill. 2012
20. Vainio H BF. Weight Control and Physical Activity IARC Handbooks of cancer Prevention. Vol. 6. Lyon: IARC. 2002
21. Webb PM. Commentary: weight gain, weight loss, and endometrial cancer. Int J Epidemiol. 2006;35(1):166-8
22. Chen Q TM, Guo F, Lau S, Zhao M. Parity Correlates with the Timing of Developing Endometrial Cancer, But Not Subtype of Endometrial Cancer. Journal of Cancer. 2015;6(11):1087 -
23. Setiawan VW, Pike MC, Kolonel LN, Nomura AM, Goodman MT, Henderson BE. Racial/ethnic differences in endometrial cancer risk: the multiethnic cohort study. Am J Epidemiol. 2007;165(3):262-70
24. Cook LS WN, Doherty JA, Chen C. Endometrial cancer: Cancer epidemiology and prevention. New York: Oxford University Press. 2006
25. Evans T, Sany O, Pearmain P, Ganesan R, Blann A, Sundar S. Differential trends in the rising incidence of endometrial cancer by type: data from a UK population-based registry from 1994 to 2006. Br J Cancer. 2011;104(9):1505-10
26. Crosbie EJ, Zwahlen M, Kitchener HC, Egger M, Renehan AG. Body mass index, hormone replacement therapy, and endometrial cancer risk: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2010;19(12):3119-30
27. Setiawan VW, Yang HP, Pike MC, McCann SE, Yu H, Xiang YB. et al. Type I and II endometrial cancers: have they different risk factors? J Clin Oncol. 2013;31(20):2607-18
28. Felix AS, Weissfeld JL, Stone RA, Bowser R, Chivukula M, Edwards RP. et al. Factors associated with Type I and Type II endometrial cancer. Cancer causes & control: CCC. 2010;21(11):1851-6
Author contact
![]() Corresponding author: Dr. Q Chen. 419 Fangxie Road, Shanghai, China. The Hospital of Obstetrics & Gynaecology, Fudan University, China. Email: q.chenac.nz; Phone: 86-13611691734
Corresponding author: Dr. Q Chen. 419 Fangxie Road, Shanghai, China. The Hospital of Obstetrics & Gynaecology, Fudan University, China. Email: q.chenac.nz; Phone: 86-13611691734

 Global reach, higher impact
Global reach, higher impact